Each and every day we learn more about COVID-19 critical illness. Sharing new findings and best practices is central to managing through this crisis. We know that progression from pneumonia to viral sepsis and ARDS is the most common scenario preceding multiple organ failure and death. ICU teams have risen to this challenge by implementing known protocols. However, we are now hearing from many centers that this is not typical ARDS. The usual strategies such as proning, low tidal volume ventilation and PEEP may be necessary, but in many cases not sufficient to get patients through this complex illness. What makes ARDS management in COVID-19 different?
RV, the forgotten ventricle.
Clinical reporting and pathology findings provide useful direction. Both ARDS-specific ventilation strategies and IV fluid resuscitation stress the right ventricle (RV) and often result in overload. Additionally, some patients exhibit left ventricular (LV) dysfunction, perhaps due to Septic Cardiomyopathy. For all of these ARDS patients, cardiovascular dysfunction is centrally important. Indeed, it appears that the RV, the forgotten ventricle, may be the main culprit in COVID-19 hemodynamic compromise.
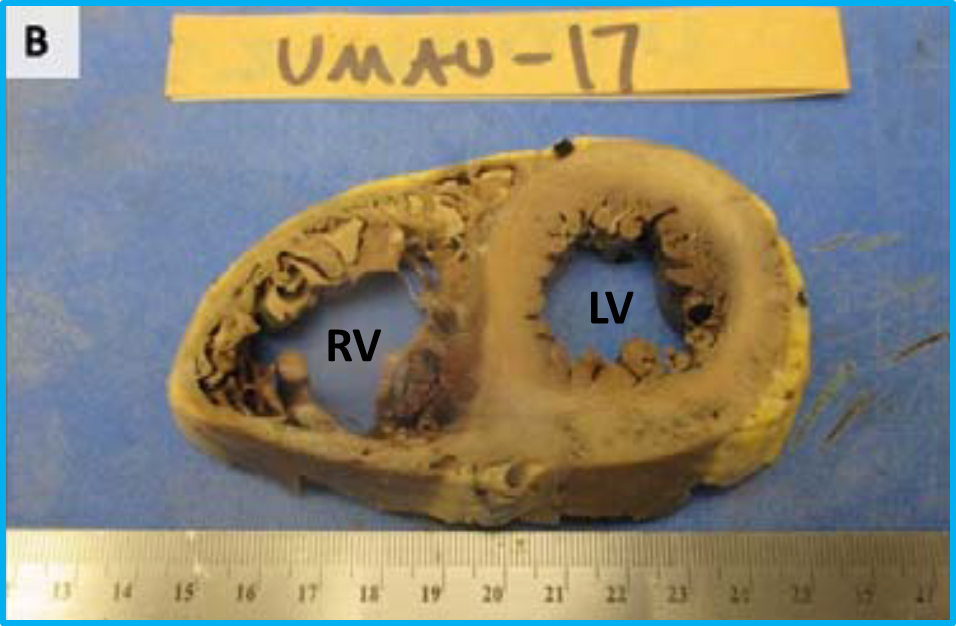
A new pathology report from the first COVID-19 autopsy series in New Orleans tells the story. All cases in this small series exhibited pulmonary edema and diffuse alveolar damage consistent with clinical ARDS. Notably, the RV was dilated in all hearts examined (3/3 cases). In fact, regarding the heart, “The most significant gross findings were cardiomegaly, and right ventricular dilatation. In one case, massive dilatation could be seen, in which the right ventricular cavity measured 3.6 cm in diameter, while the left ventricle measured 3.4 cm in greatest diameter.”[1] Normally the RV is less than 2/3 the size of the LV.
We already knew that the RV could be affected in ARDS management, and now we know it’s even more important in these critically ill patients. As COVID-19 is a systemic illness, what else is making this so difficult to manage?
Vascular abnormality, too?
The New Orleans pathology report highlights a new and unexpected finding. In addition to ARDS and RV dysfunction, there is a vascular abnormality. “Important additional mechanisms that may have contributed to death in this initial series of autopsies include a thrombotic microangiopathy that was restricted to the lungs.”[1] Outside of COVID-19, finding thrombotic microangiopathy in the lungs is very unusual. This speaks to a fundamental cardiovascular effect that may contribute further to the difficulty in managing these patients. Many centers are finding that some form of anticoagulation is necessary. What we have here is an “atypical” form of viral sepsis with ARDS, in that RV dysfunction and microvascular thrombosis are complicating factors.
Not so easy.
Conventional hemodynamic monitoring using volume responsiveness methods cannot provide accurate guidance in the face of RV dysfunction. These indirect methods are dependent on both normal heart lung interaction and normal RV function. Such noninvasive monitors indicate the need for more fluid when in fact that may be the opposite of what is actually needed when the RV is already overloaded.[2] We cannot afford to get this wrong and further stress the RV in COVID-19 ARDS patients.
So what can we do?
Since we now know that RV management plays a vital role in reducing the unbearably high mortality rate, why not look at the RV directly? ImaCor’s Hemodynamic Ultrasound has played a vital role in the care of more than 20,000 intubated patients to date. Using ultrasound, this method uncovers RV dysfunction at its inception, helping you to avoid RV failure. Indeed, Hemodynamic Ultrasound is the only way to effectively manage the RV at the bedside over a period of time in the ICU. While transthoracic echo may be available, surface ultrasound is best suited to screening and not management of unstable, intubated patients. The ClariTEE probe can be left indwelling for up to 72 hours for repeatable and reproducible assessments, which can be done by front line providers. It is safe, easy to use, and purpose-built for this specific environment. We can help you manage these patients with actionable information vitally important for these severely ill COVID-19 patients.
Novel critical circumstances demand bold and direct solutions. COVID-19 ARDS patients with exceedingly high mortality rates need action now. Let us help you manage patients through these exceedingly difficult times.
Share this, call us – we’re here for you.
[1] Fox S, Akmatbekov A, Harbert J, et al. Pulmonary and Cardiac Pathology in Covid-19: The First Autopsy Series from New Orleans. MedRxiv 2020.04.06.20050575. https://doi.org/10.1101/2020.04.06.20050575
[2] Miller A, Mandeville J. Predicting and Measuring Fluid Responsiveness with Echocardiography. Echo Res Pract. 2016;3(2):G1–G12. https://doi.org/10.1530/erp-16-0008