To our community of critical care colleagues and front line service providers:
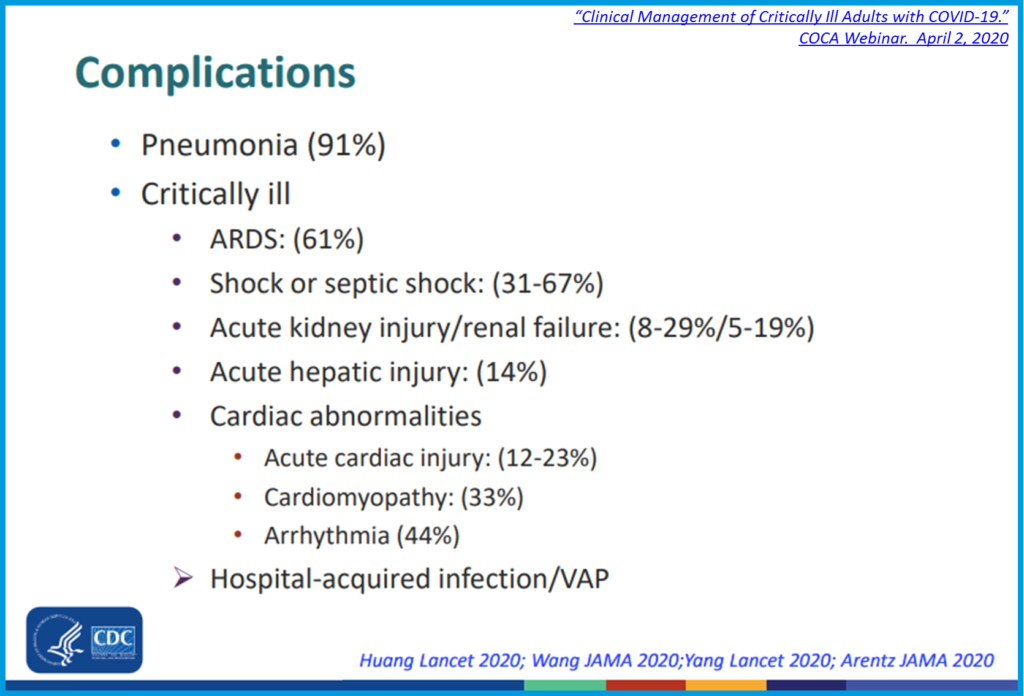
ICU patient management has never been easy. Faced with an unprecedented influx of critically ill COVID-19 patients, sharing best practices has never been more important. Most COVID-19 fatalities are due to severe pneumonia and inflammation complicated by ARDS and multiple organ failure. Early data from US hospitals indicate that 20-40% of COVID-19 ICU patients have ARDS, mirroring reports from China and Europe. Indeed, over 50% of COVID-19 ICU patients with ARDS succumb to the disease.[1] This is too deadly to ignore.
Mechanical ventilation alone is not enough to manage these complex patients.
 Simultaneous respiratory and cardiovascular support is mandatory. Unfortunately, ARDS-specific ventilation strategies and IV fluid resuscitation both stress the RV and often result in overload. Unrecognized RV dysfunction prolongs time on vent, increases ICU days, and contributes to excess mortality. Stress cardiomyopathy, both initially and at resolution of the disease process, has also been found to contribute to all-cause mortality.
Simultaneous respiratory and cardiovascular support is mandatory. Unfortunately, ARDS-specific ventilation strategies and IV fluid resuscitation both stress the RV and often result in overload. Unrecognized RV dysfunction prolongs time on vent, increases ICU days, and contributes to excess mortality. Stress cardiomyopathy, both initially and at resolution of the disease process, has also been found to contribute to all-cause mortality.
Since the RV simply cannot be assessed and managed using conventional monitoring, additional capability is required. Screening tools such as surface echocardiography can be helpful in non-intubated patients. However, for continuous management of complex intubated patients, snapshot surface ultrasound is inadequate as a primary tool.
We have found that continuously available Hemodynamic Ultrasound (or “hTEE”) is a safe, effective, and easily deployable tool. Specifically created to monitor LV preload and RV function over time, the single patient use ClariTEE probe can remain indwelling for up to 72 hours. These disposable, single use ultrasound probes promote patient and provider safety, with a consistent track record in over 20,000 intubated patients on mechanical ventilation.
Hemodynamic Ultrasound is particularly useful in managing RV dysfunction.[2] Since RV function correlates with ventilator days[3] we can expect this visually guided management will help to reduce time on the ventilator for COVID-19 patients with ARDS. It will help us preserve ICU and ventilator capacity. Most importantly, we know that patients who are weaned off of mechanical ventilation sooner experience better outcomes and less mortality. Throughout our country, “COVID-19 patients are hooked on a ventilator for anywhere from 10 days to 21 days – with a high death rate.”[4] Reducing ventilator time can shift the survival probability in favor of the COVID-19 patient while achieving the added benefit of making a limited resource, the ventilator itself, available to more patients.
We need to act now to reduce ventilator days and avoid as many fatalities as possible.
We strongly support strengthening your efforts to fight the virus by adopting Hemodynamic Ultrasound as a best available practice in guiding the management of the most complex intubated COVID-19 patients. We can save lives together as we provide critically needed supportive care of ARDS and multisystem failure. Doing so will maximize available resources for these most vulnerable patients.
Please join with us in sharing these best practices to win the fight against this outbreak in our communities. Most assuredly we can rise to this new challenge together.
Sincerely,
Scott L. Roth MD FACC
CEO, ImaCor Inc.
Critical Care Leadership:
- Margarita Camacho MD FACS
- Nicholas Cavarocchi MD
- Subbarao Elapavaluru MD
[1] Wu C, Chen X, Cai Y, et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. Published online March 13, 2020. doi:10.1001/jamainternmed.2020.0994
[2] Fletcher N, Geisen M, Meeran H, Spray D, Cecconi M. Initial clinical experience with a miniaturized transesophageal echocardiography probe in a cardiac intensive care unit. J Cardiothorac Vasc Anesth. 2015;29(3):582–587. doi:10.1053/j.jvca.2014.09.016
[3] Younan D, Pigott DC, Gibson CB, Gullett JP, Zaky A. Right ventricular fractional area of change is predictive of ventilator support days in trauma and burn patients. Am J Surg. 2018;216(1):37–41. doi:10.1016/j.amjsurg.2018.02.002
[4] https://nypost.com/2020/03/29/heres-the-next-big-problem-after-new-york-gets-ventilators/