ImaCor’s Hemodynamic Ultrasound Method uses many of the same gold-standard TEE practices performed in surgery.
Both produce high-quality images of a patient’s heart, but Hemodynamic Ultrasound is far less complicated, the equipment far less expensive, and requires limited training. And it’s never been more important to use post-operatively for your most critically ill patients.
Why Hemodynamic Ultrasound has never been more important
Today’s ICU population is increasingly comprised of complex patients with multiple co-morbidities. They require advanced hemodynamic management because even a brief period of hemodynamic instability can lead to life-threatening complications, lengthy stays, negative outcomes, and high costs (Zenati MS, et al. J Trauma, 2002). Older, sicker patients with multiple co-morbidities:
- Linger in the ICU
- Don’t respond to treatment
- Extend ICU length of stay
- Consume a disproportionate share of resources
“The Fluid Challenge” is so yesterday
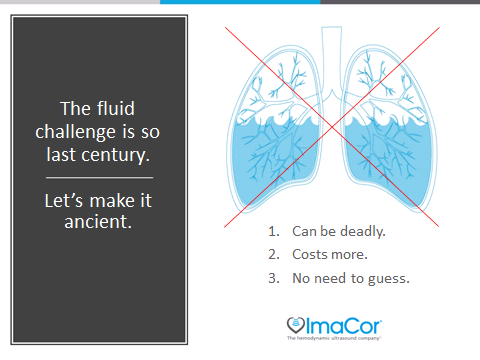
If you want to break the cycle of hemodynamic instability, you’ve got to move beyond the indirect parameters you’re using today (urine output, blood pressure, lactate, and cardiac output). These indirect methods provide little insight into true cardiac performance. In fact, they can mislead you when managing complex patients, forcing you to guess which therapy would yield the best outcomes.
You’re surely familiar with the “fluid challenge.”
In the absence of simultaneously observing and measuring real-time cardiac filling and function, your hemodynamic management technique may be little more than trial-and-error.
For example if your patient is hypotensive, and you don’t have direct visualization of the heart, you don’t know if the cause is hypovolemia, myocardia dysfunction, vasodilation, or any combination of them.
So you perfuse, challenging the body with as much fluid as it can process, potentially flooding the patient with fluids she can’t absorb.
As we said, that’s so yesterday.
See first. Then intervene.
With today’s Hemodynamic Ultrasound hTEE technology, why guess when you can see preload and contractility, RV and LV size and function, and volume responsiveness before you intervene?
See these amazing statistics from peer-reviewed studies of the hTEE method:
• hTEE made a direct, therapeutic impact in 66 percent of patients (Vieillard-Baron)
• hTEE reduced the use of continuous renal replacement therapy (CRRT) by 50 percent (Griffin)
• Using hTEE, RV failure was diagnosed in almost 70 percent of patients (Fletcher)
Here’s how it works: