Hemodynamic Ultrasound™ is the platform that enables direct visualization of cardiac filling and function over time to guide patient management for critically ill patients.
Why is Hemodynamic Ultrasound so important?
Because, for your highest-risk patients, hemodynamic status may change dramatically in a matter of minutes – and potentially while you’re waiting for test results you submitted 15 minutes ago. Yes, in that time, your septic patient might have benefited from increased inotropic support. Or a vasopressor. Or a mechanical ventilation adjustment.
In the TEE and TTE family
Your hospital has used diagnostic ultrasound for years: Both transesophageal echos (TEE) and transthoracic echos (TTE) are forms of diagnostic ultrasound. Transesophageal echo, is argued by Hwang, Porembka, Vignon, and many others, to be the stronger of the two modalities. What’s more, accurate transthoracic assessments are hard to come by: Limited acoustic windows and body habitus get in the way.
Transesophageal echo and transthoracic echo are most commonly used during vascular and cardiac surgeries. It’s what happens after surgery where opportunity lies for you to reduce time, complications, and resources.
And that, my friends, is the reason we exist.
Hemodynamic Ultrasound for critical care
Until recently, it’s been wildly impractical to use conventional transesophageal echo for any length of time in the critical care setting. Conventional transesophageal probes are too big to stay indwelling, and the case cost tying up a TEE machine for days is intolerably high.
Today a newer Hemodynamic Ultrasound modality is available. It’s called the hTEE method and it’s designed specifically for your most at-risk patients in critical care.
Using a disposable hTEE probe the size of an NG tube that can stay indwelling for 72 hours, now you can directly track cardiac activity via the transgastric short axis, midesophageal four chamber, and superior vena cava views.
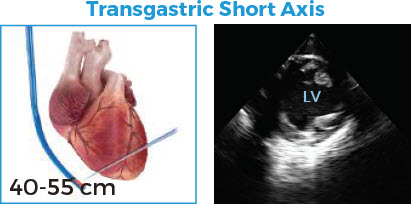

Goal
• Assess preload and contractility
Technique
• Advance probe past gastroesophageal junction into stomach
• Anteflex to optimize contact
• Image at the mid-papillary level
Assessment
• Preload using LV size and LVEDA measurement
• LV contractility using FAC calculation
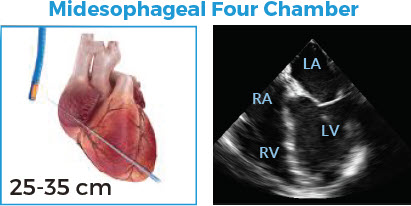

Goal
• Evaluate ventricular size and function
Technique
• Position probe just below aortic valve
• Retroflex to visualize four chambers in long axis
Assessment
• Relative size of RV and LV in diastole
• Left ventricular systolic function
• Right ventricular systolic function
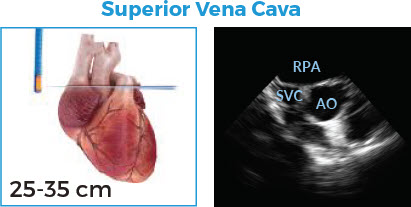
Goal
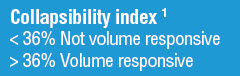
• Assess volume responsiveness
Technique
• Position probe above the aortic valve
• Visualize SVC adjacent to the ascending aorta
Assessment
• SVC size and collapsibility
It’s so much better than the trial-and-error approach found in so many institutions.
And there’s money in it too.
We know. It’s uncouth to bring economics into a proper conversation about improving patient outcomes.
But unless your hospital is convinced Hemodynamic Ultrasound is clinically superior AND economically feasible, it ain’t gonna happen.
Well, Hemodynamic Ultrasound is economically feasible. And here is the solid economic case for bringing Hemodynamic Ultrasound to your institution.
1Intensive Care Med 2004; 30: 1734-1739 2Am J Respir Crit Care Med 2003; 168:1270-1276