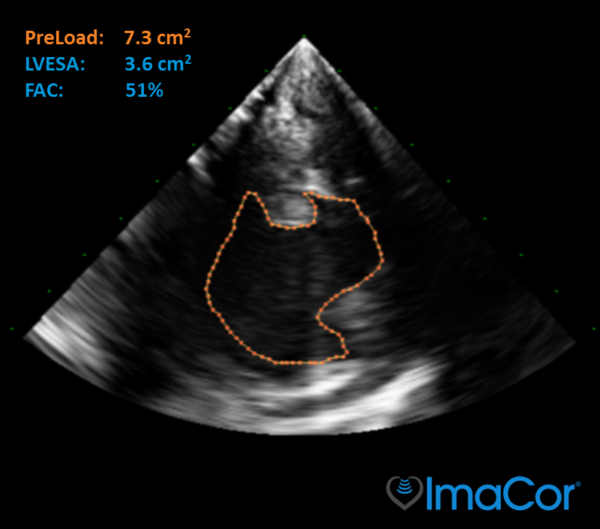
It’s the holy grail for ICU fluid management.
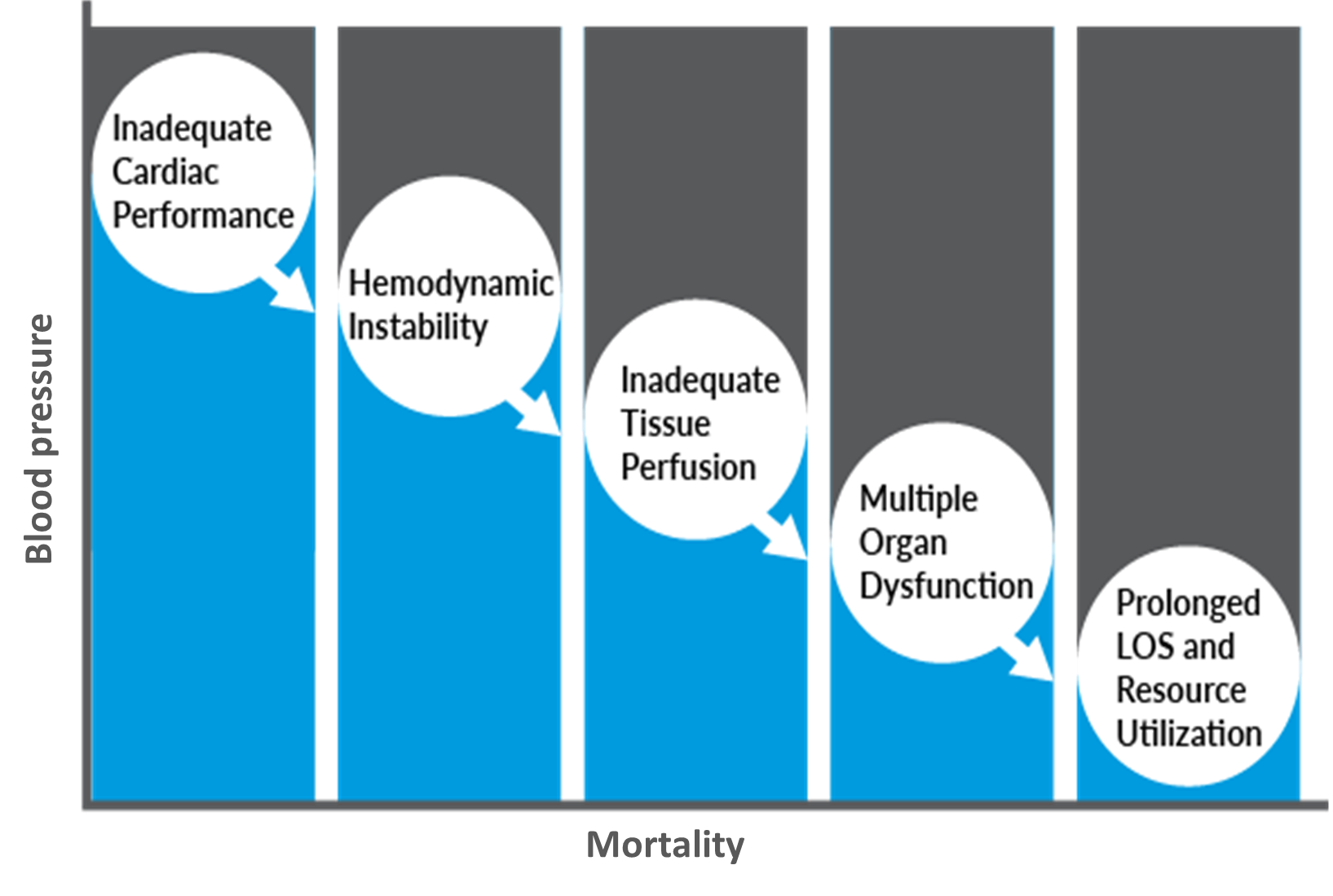
You get called in because the patient’s Blood Pressure (BP) is low. Should you give fluids? BP, urine output, lactate, and cardiac output numbers are available, but these indirect methods provide little insight into cardiac performance and can be misleading targets for resuscitation.
Without knowing Preload right then and there, you are forced to make a decision and direct fluid therapy based on inadequate information. Without knowing if RV function is normal or not, just pushing volume may cause more harm than good.