Background
71 year old woman with a history of cigarette smoking, type II diabetes, possibly previous diagnosis of CHF is transferred from a secondary hospital where she was admitted 3 days prior for shortness of breath and fever and a diagnosis of community acquired pneumonia. Antibiotics were started but she worsened and required intubation. Dopamine was started after intubation to support her blood pressure.
On arrival at FMC, patient’s BP was labile, on dopamine 10 ug/kg/min and ventilator, acceptable urine output.
Method
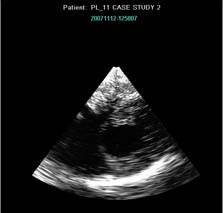
A miniaturized bedside TEE exam was conducted using th ClariTEE probe. The probe was easily passed and a transgastric short axis view (TGSAV) of the left ventricle was obtained.
Patients’s heart looks underfilled and a fluid bolus is suggested and given. Patient’s BP less labile and dopamine is weaned to 6 ug/kg/min overnight.
 Day 2 in the a.m:
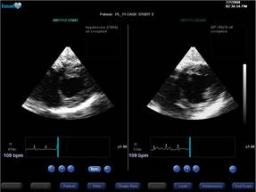
Day 2 in the a.m:
The patient was awake and interactive. HR 79 BP 105/55, CVP 10 with ventilator settings unchanged. Urine output however was low…..just under 30 cc/hr. The heart still looks underfilled and more pentaspan given (500cc). Dopamine was weaned off over the next 3 hours and urine output is better (over 100cc/hr). CVP rises to 16.
Patient was extubated on Day 3, out of the ICU on Day 4, and out of hospital on Day 9.