Case presented in an invited faculty lecture at the TJU hTEE course, May 16, 2013.
The Patient
A 72 year old male pedestrian was stuck by a motor vehicle and suffered multiple severe orthopedic injuries: fractures of both lower extremities, an acetabulum, ribs, and spinal column fractures. As a result, he suffered severe deconditioning resulting in ventilator-dependent respiratory failure and required a tracheostomy. The patient was ultimately discharged to a long term acute care hospital (LTACH) after several weeks.
Re-admission to Hospital
The patient was subsequently readmitted for increasing anasarca, progressive hypotension, and hypoxia. He was presumed to have septic shock, likely of pulmonary origin. He met criteria for ARDS. He quickly required multiple pressors (neosynephrine, norepinephrine and vasopressin) and developed high mean airway pressures.
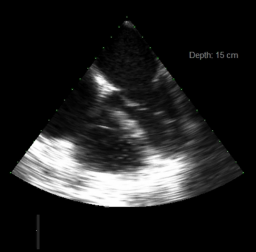
Echocardiography History
An echocardiogram during the previous admission had revealed a slightly reduced ejection fraction (35-40%), moderate to severe LV hypertrophy, and normal RV size and function.
Why hTEE?
The patient suffered progressive oliguria from sepsis-induced acute kidney injury. He continued to have severe anasarca, and had a CVP of 20 mmHg. The patient was initially given lasix, a standard treatment for anasarca and pulmonary edema seen on chest x-ray, but he did not respond. TTE was not possible due to absence of windows (body habitus, ventilator settings and anasarca). hTEE was therefore placed.
hTEE Results
hTEE revealed a depressed and under-filled LV, and a moderately dilated RV with severely depressed function, significantly worse as compared to his previous admission’s echocardiogram.