Is hypotension as harmful to critical care patients as was feared?
If you embrace this study by Kamal Maheshwari, et. al., the answer is an emphatic yes, perhaps even more than previously thought.
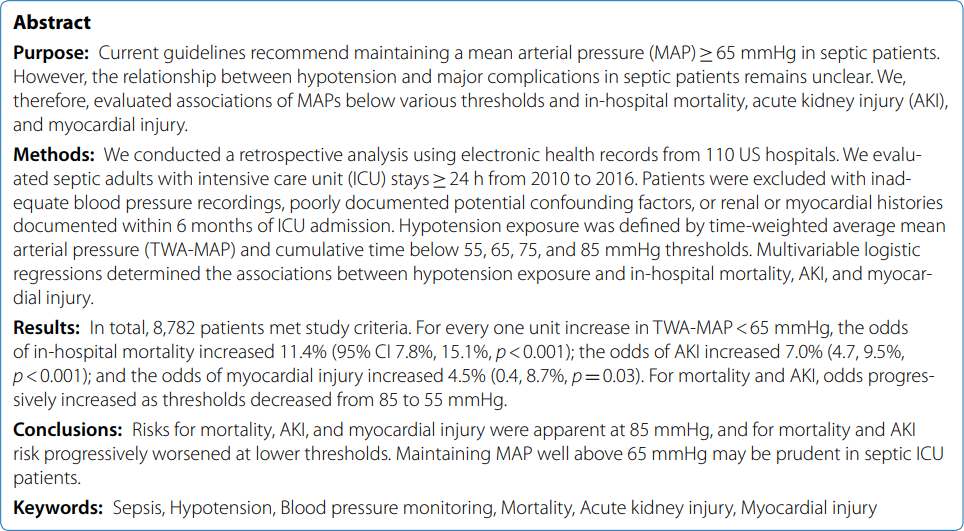
His team tested the current mean arterial pressure (MAP) guideline – maintain MAP above 65 mmHg in septic patients – by retrospectively analyzing electronic health records from 110 hospitals, observing associations of MAPs below various thresholds and in-hospital mortality, acute kidney injury (AKI), and myocardial injury.
 Looking at time-weighted average mean arterial pressures (TWA-MAPs), they conclude:
Looking at time-weighted average mean arterial pressures (TWA-MAPs), they conclude:
For every unit TWA-MAP falls below 65 mmHg,
- the odds of in-hospital mortality increased 11.4% (95% CI 7.8%, 15.1%, p<0.001);
- the odds of AKI increased 7.0% (4.7, 9.5%, p<0.001); and
- the odds of myocardial injury increased 4.5% (0.4, 8.7%, p=0.03).
Below 85 mmHg?
Maheshwari’s conclusions go far beyond the current 65 mmHg guideline, saying, “Risks for mortality, AKI, and myocardial injury were apparent at 85 mmHg.” He noted mortality and AKI
risk progressively worsened at lower thresholds.
The medical community already knew about the gravity of sepsis. In 2008 alone, nearly $15 billion was spent in the US treating sepsis more than a decade ago! (If you know the current number, please let us know.)
Much of the end-organ damage to patients were consequences of hypoperfusion.
Implication for you
It’s likely you already check MAP using an arterial line. You can do more for your patient.
Instead of relying solely on MAP as an indicator of adequate perfusion, hemodynamic ultrasound shows you – in real time – if the patient has adequate LV pre-load and LV function necessary to maintain MAP goals. Namely, directly seeing heart filling and function can help you achieve your MAP goals.
Then, once you start adding fluid or pharmocologic agents to improve function, hemodynamic ultrasound shows you heart filling and function in real time.
Showing you heart performance in real time is kind of why we exist. So if you’ve not yet adopted the ImaCor hemodynamic ultrasound system, here’s yet another study suggesting you do.
Contact us today for a no-obligation demonstration, won’t you?