The Patient
A 55-year-old male with a 3 day history of a perirectal abscess, which had been drained 2 days prior, presented with 24 hours of excruciating discomfort, nausea and vomiting that had been worsening over time. At admission, the patient was afebrile with low-grade tachycardia. The examination was significant for erythema and induration of the bilateral gluteal region, perianal bullae and a fluctuant area at the 6 o’clock position. Laboratory results indicated the patient had acute kidney injury and was volume depleted. The patient was admitted to the ICU for active resuscitation, intravenous antibiotics, and then taken emergently to the operating room for debridement of the necrotizing soft tissue infection involving the groin and ischiorectal fossa.
STICU Admission and Course
The patient was admitted to the STICU post-operatively in critical condition with acute respiratory failure, acute renal failure, and septic shock requiring fluid administration and vasopressor agents. A return trip to the operating room was undertaken the following day for further debridement and a transverse loop colostomy. Over the next few days the urine output improved, vasopressors were weaned, and antibiotics were tailored to the E.coli and Enterococcus found on wound culture. The patient was extubated seven days into the hospital stay and was tolerating tube feedings at goal.
On Hospital day #13 laboratory results demonstrated an elevating white blood cell count associated with increasing fever. After the most recent trip to the operating room for wound evaluation, debridement and dressing change, the patient remained intubated; consistent with his worsening physiologic status. Antibiotics were expanded to a broader spectrum and a CT scan of the abdomen and pelvis revealed new fluid collections along the bilateral abdominal walls and sacrum. A return trip to the operating room for debridement and drainage of the new CT findings ensued. Post-operatively the patient was in septic shock with hypotension, tachycardia, acute renal failure, and respiratory failure.
Hemodynamic Management and Assessment pre-hTEE
Vasopressors were initiated and a right subclavian central venous catheter was placed with an initial central venous pressure of 19 mmHg which may have been interpreted as having adequate intravascular volume. A decision was made to insert an hTEE probe to better assess the patient’s volume and cardiac status.
Initial hTEE Assessment and Resuscitation
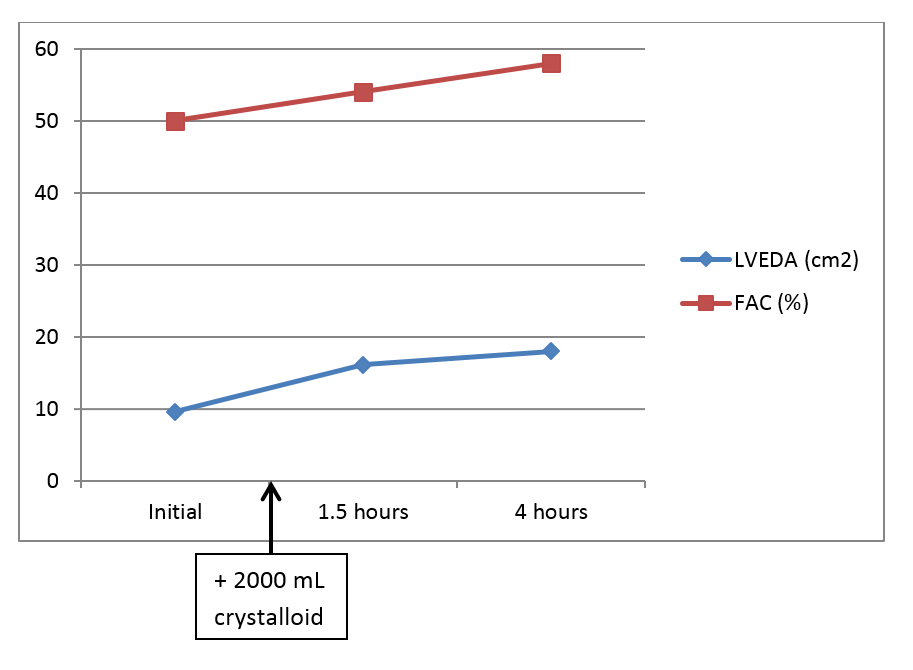
Upon initial insertion of the probe there was great difficulty obtaining the SVC view which appeared to be collapsed. Therefore, we moved on to the TGSAV and the ME4Ch views. The patient’s heart appeared to be isodynamic with no wall abnormalities and an initial FAC of 50%. The LVEDA measured from the TGSAV was 9.6 cm2. With the apparent inadequate preload and adequate cardiac function two liters of crystalloid solution were infused.
Subsequent hTEE Assessment and Management
Repeat hTEE exams performed at 1.5 hours and 4 hours showed an improved LVEDA over time from 16.1 cm2 to 18 cm2and FAC of 54% to 58% respectively. Despite an adequate LVEDA, this patient required vasopressors to maintain end organ perfusion. The patient appeared to remain volume responsive following our data points. As LVEDA increased so did the FAC; very much like a Frank-Starling curve.
Continued hTEE-guided Resuscitation
One liter of 5% albumin was infused and the SVC index, which was now measurable, improved to 0.37 while the vasopressor infusion decreased. The LVEDA at this point remained 18 cm2 with an FAC of 56% and non-collapsible right ventricle on ME4Ch view. Twelve hours into this resuscitation the patient had received a total of 2000 mL of crystalloid, 1000 mL of albumin, 1 unit of packed red blood cells and the vasopressors were nearly off. Interestingly the CVP at the beginning of the resuscitation was 19 mmHg and 12 mmHg following the previously mention fluid administration. At 24 hours the SVCi was 0.28, LVEDA 17.5cm2, and FAC 51% with a non-collapsible SVC and no vasopressor support.
 Discussion
Discussion
How are we to understand the drop in CVP from 19 mmHg before volume resuscitation to 12 mmHg following the administration of three liters of fluid? A possible explanation may be found in Marik et al. (2011): The CVP is a good approximation of right atrial pressure, which is a major determinant of right ventricular (RV) filling. It has been assumed that the CVP is a good indicator of RV preload. Furthermore, because RV stroke volume determines LV filling, the CVP is assumed to be an indirect measure of LV preload. However, due to the changes in venous tone, intrathoracic pressures, LV and RV compliance, and geometry that occur in critically ill patients, there is a poor relationship between the CVP and RV end-diastolic volume. Furthermore, the RV end-diastolic volume may not reflect the patients’ position on the Frank-Starling curve and therefore his/her preload reserve.
Conclusion
The hTEE allowed the STICU team to manage this patient with septic shock more appropriately by assessing the adequacy of the patients’ volume status through utilizing the SVC index, LVEDA and FAC in a dynamic fashion.
Reference
Marik PE, Monnet X, Teboul JL. 2011. Hemodynamic parameters to guide fluid therapy. Ann Intensive Care 1:1. doi: 10.1186/2110-5820-1-1.